Researchers unearth new bacteria-resistant antibiotic
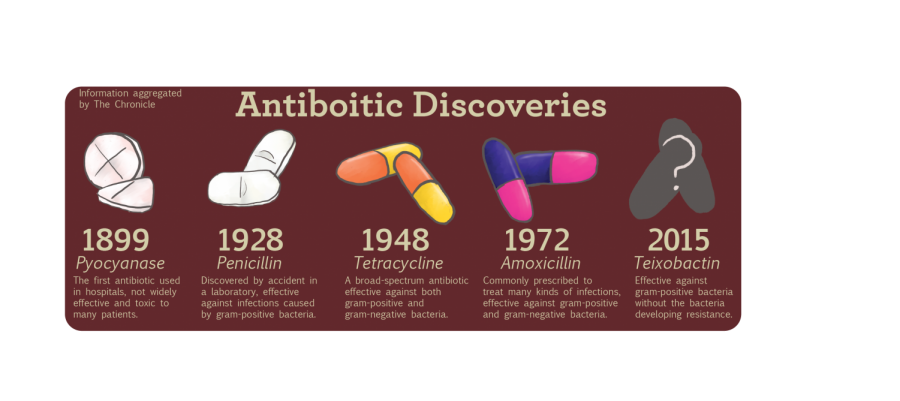
Antibiotic Discoveries
January 26, 2015
Scientists have searched for ways to combat antibiotic-resistant bacteria for nearly 30 years, but it turns out the answer may have been under their feet the entire time.
Researchers from Northeastern University in Boston have discovered a new antibiotic called teixobactin by developing a novel extraction device called the iChip, which grows bacteria in soil.
“It was discovered over a hundred years ago that the majority of cells in nature would not grow in the lab,” said Slava Epstein, a professor of microbiology at Northeastern. “It’s not clear why they wouldn’t grow, but the more practical question was, ‘Can we [grow it]?’ If we grow microorganisms in their natural environment, [it will] provide the cell with growth factors that are found in [its] habitat.”
According to the study, published Jan. 7 in the journal Nature, teixobactin successfully killed strains of gram-positive bacteria that cause infections, including strep throat, anthrax and staph infections.
“There is one limiting factor to teixobactin, and that is that it only hits gram-positive organisms,” Conlon said. “A lot of our resistance issues today are with the multi-drug resistance evolution that we are seeing in some gram-negative pathogens. As things stand, teixobactin will not be capable of hitting the majority of those.”
According to Mark Mandel, assistant professor of microbiology at Northwestern University, the use of the iChip is a breakthrough in itself.
“One thing that is really impressive and that led to the initial discovery was the focus on using uncultured bacteria and studying them starting in their natural habitat,” Mandel said. “This paper presented a new technology that was really promising by actually letting [the bacteria] have access to the nutrients of their natural environment while still giving them an enclosed place to grow.”
Researchers are optimistic about the development of teixobactin because it speedily kills pathogens and blocks the bacteria from reproducing, according to the study. In initial trials on mice, teixobactin showed no signs of developing a resistance to bacteria.
“What really makes it interesting is that lack of any detectable [bacterial] resistance to this compound,” said Brian Conlon, co-author of the study and a senior scientist at Northeastern’s Antimicrobial Discovery Center. “Usually when we find an antibiotic and you put it through some rigorous testing, you’ll detect some resistance. We predict it will take at least 30 years of heavy chemical use for that resistance to emerge.”
If the antibiotic is developed into a clinical drug, it could help combat the antibiotic-resistance crisis. According to a 2013 threat report by the Centers for Disease Control and Prevention, at least 23,000 Americans die annually of infections that have developed a resistance to antibiotics. The Review on Antimicrobial Resistance, led by economist Jim O’Neill, found that by 2050, as many as 10 million people could die per year of previously curable infections if bacteria continue to evolve at the current rate. Researchers are hopeful that the pharmaceutical development of teixobactin could fight infections that have built up a resistance to current antibiotic treatments, such as tuberculosis.
“Resistance has been evolving and strains have been detected—[there are people who] are resistant to all of the conventional antibiotics used to treat tuberculosis,” Epstein said. “That’s huge, especially when you consider tuberculosis kills three million people a year. If it continues to evolve at this rate, we will need new drugs to fight TB.”
Before FDA approval, teixobactin will have to endure rigorous testing and trials. According to Epstein, it could take 5–10 years before the drug is available.
“There are many steps and many barriers that this molecule will have to overcome on its way to the shelves,” Epstein said. “It’s not that those barriers exist only for teixobactin—anything will have to show its performance at different levels before becoming a drug. If it is successful at all of those steps, then yes, in that many years, it may end up being used. It’s an optimistic view—not unrealistic, but optimistic at the same time.”
Epstein said the method of teixobactin’s discovery could pave the way for similar breakthroughs.
“While there is every reason to be optimistic, realistically speaking, we don’t have a drug,” Epstein said. “There is, though, every reason to be optimistic about the future. The mere fact is we have a pipeline of microbial diversity that, together with novel compounds, makes me hopeful that eventually we will get a new antibiotic and perhaps other pharmaceuticals.”