Cholesterol exonerated, maybe
Cholesterol exonerated, maybe
March 2, 2015
Two sunny side up eggs and a strip of bacon graced the cover of Time magazine in March 1984, forming the distressed, frowning caricature of a human face. The message imparted to the American people by this proto-emoji was simple: Ditch dietary cholesterol to dodge heart disease.
However, recent research—including analyses of many early studies that may have mistakenly established a link between cholesterol in the diet and coronary artery disease—has slowly mustered an appeal for dietary cholesterol, at least enough so that the Dietary Guidelines Advisory Committee has taken notice.
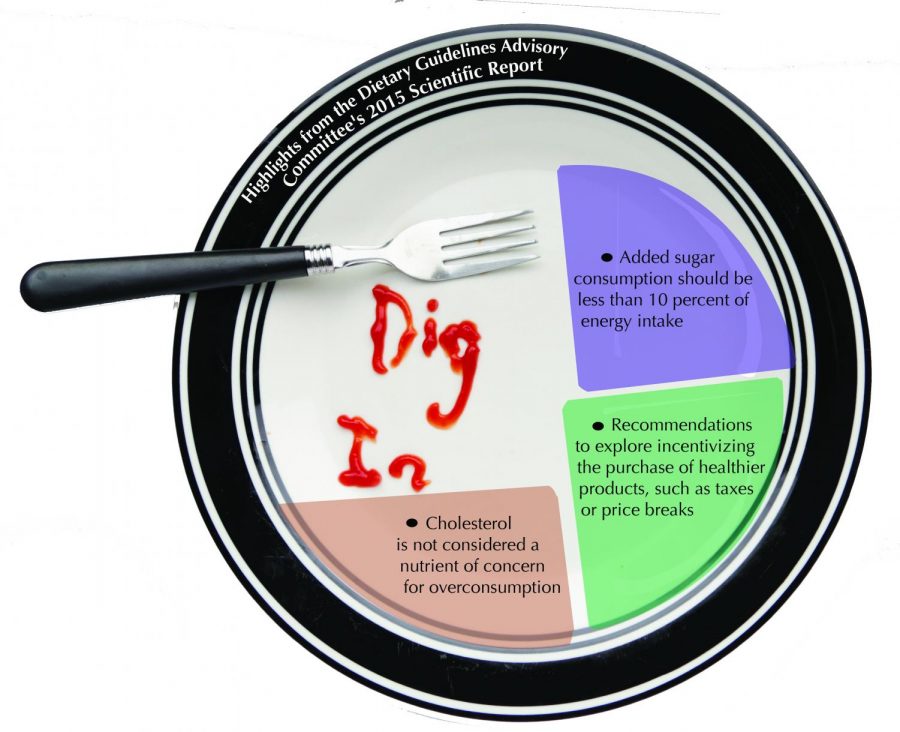
The United States Department of Agriculture and the Department of Health and Human Services determine dietary recommendations for the American public based on a scientific report published every five years by the DGAC. Among other changes, the 2015 report declared “Cholesterol is not a nutrient of concern for overconsumption,” effectively abolishing the recommendations that have served as a linchpin of medical practice for half a century.
The pre-existing recommended daily allowance for cholesterol, enacted in 1977, was 250–300 milligrams—two eggs clock in at about 375 milligrams.
“We reviewed the literature, and cholesterol was one of those guidelines that has just been kept,” said Alice H. Lichtenstein, professor of nutrition science and policy at Tufts University and vice chair of the 2015 DGAC. “The effect of dietary cholesterol in isolation was actually quite small, there was no reason to carry it forward.”
Subcommittees of DGAC members formulate specific questions after reviewing the prior report and determine which areas of diet, health and nutrition need to be re-reviewed because new data may have been generated, according to Lichtenstein. She said the new research has indicated that the biomarkers that indicate a risk factor for cardiovascular disease are more closely related to the types of fat ingested, such as saturated or polyunsaturated, rather than cholesterol—a waxy, fat-like substance naturally produced in the human body and found in cell membranes.
“The cholesterol molecule is one of the most important ones we have in our body,” said Dr. Uffe Ravnskov, an independent investigator who has spent decades researching the link between diet and heart disease. “The highest cholesterol concentration is saturated in the brain—you can’t think without producing cholesterol in the brain every second.”“The highest cholesterol concentration is saturated in the brain—you can’t think without producing cholesterol in the brain every second,” Ravnskov added.
Ravsnkov said he used to call the medical establishment’s campaign against dietary cholesterol the “greatest medical scandal of modern times,” but the reasons for the long-standing vilification of saturated fat and cholesterol in the diet are complex and rooted in both human psychology and economics. Once an idea—like the cholesterol-heart hypothesis—gains traction in the scientific community during the course of nearly 50 years, it can be a challenge for researchers to view new data or the results of re-examined data in an unbiased light. It can also be difficult to garner funding for studies that call into question ideas that have existed for so long that they have become cemented in the minds of researchers as fact.
“One thing is for sure, [the cause of heart disease] is not cholesterol,” Ravnskov said.
The journal Open Heart published a meta-analysis in December 2014 of all of the randomized controlled trials conducted prior to 1977 that were used as evidence for the original USDA cholesterol recommendations. Fergal Grace, a reader in physical exercise physiology at the University of the West of Scotland and co-author of the study, said there had never been a re-evaluation of the data that formed the basis of cholesterol’s initial and enduring condemnation.
“We’re looking through a telescope, looking at the evidence available at that time,” Grace said. “Having run [the analysis], it turns out that there was no effect really. It really sat on the zero line, and the zero line says it doesn’t favor the control group or the intervention.”
Dietary studies in particular are notoriously difficult to run because they are conducted over long periods of time and many unsuspecting factors can influence the results. One of the major confounders is the goal of looking at the role a single nutrient can play in the body. For example, if a study participant is replacing fat with carbohydrates, or carbohydrates with proteins, total energy intake is not taken into account. The original thought behind the cholesterol-heart hypothesis was that cholesterol in food would increase cholesterol in the blood, and this would lead to greater risk of death from cardiovascular disease, he said.
“The best [data available showed] that there wasn’t randomized controlled trial evidence that would support the introduction of the dietary guidelines,” Grace said.
Lichtenstein said in addition to the new recommendations regarding cholesterol intake, the 2015 committee reviewed new scientific literature relating to coffee and caffeinated beverages as well as focusing heavily on consumers’ dietary patterns. An emphasis was also placed on environmental sustainability in food production.
“We felt it was important to emphasize that one should always consider the whole dietary package and not just individual foods or nutrients,” Lichtenstein said. “When one thing goes up in terms of food, something else goes down. Even if you consume the highest quality diet and it’s in excess of energy needs, you will gain weight and you won’t gain the benefit of those healthier choices. Whatever is said, it needs to be in the context of achieving and maintaining a healthy body weight.”