Metabolic shift in cells key to threat recall
Metabolic shift in cells key to threat recall
October 6, 2014
New research from the Geisel School of Medicine at Dartmouth College in New Hampshire suggests that the ability of the innate immune system’s cells to remember and fight off specific threats may be connected to a particular genetic pathway that determines how they metabolize energy.
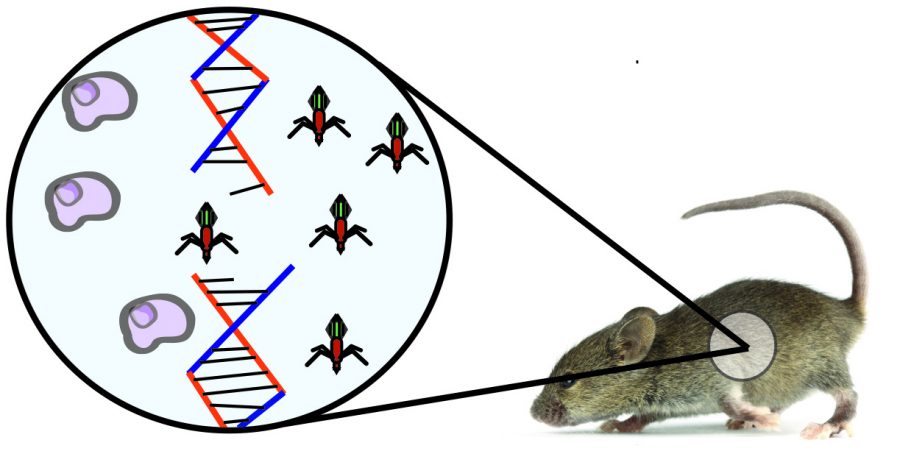
The study, published Sept. 26 in the journal Science, looked at mice that had the gene HIF1-alpha, hypoxia-inducible factor 1-alpha, deleted from their innate immune system cells. HIF1-alpha plays a role in energy metabolism in immune cells. The mice were exposed to a fungal antigen, beta glucan, to induce and sustain a trained immune response. Following the first exposure, they were then presented with a second threat in the form of a bacterial pathogen. Mice with unaltered genetics were able to fight off the secondary attack normally, but mice without HIF1-alpha were not.
Researchers concluded the missing gene might be essential for the trained cells to undergo the metabolic shift, the lack of which left them vulnerable to the pathogen. This shift seems to affect the cell’s epigenetics—changes in how the genes within the cells are being expressed without altering the genetic code itself—locking the cells in the trained state.
“When our collaborators in the Netherlands first did the epigenetic profiling of the trained versus the non-trained cells, they identified certain genes that were predicted to be important in the subsequent response of these trained cells,” said Robert Cramer, a researcher involved with the study and an assistant professor of fungal pathogenesis at the Geisel School of Medicine.
According to Cramer, a naive cell—one that has not encountered a molecular pattern from a pathogen that it would recognize and remember as a threat—uses a process of energy generation called oxidative phosphorylation. After that cell recognizes a molecular pattern from a pathogen or virus, it begins to use a process called aerobic glycolysis to generate its energy.
“With the trained cells, what we’re observing is that when they are exposed to molecular patterns [from pathogens], not only does it initiate an immediate and non-specific broad type of response [from the adaptive immune system], but these cells are actually able to then remember that they’ve been exposed to these pathogen molecular patterns and they do this by changing their metabolism,” Cramer said.
According to David Fruman, professor of molecular biology and biochemistry at the University of California, Irvine’s School of Biological Sciences, the immune system is divided into two components: the innate response that is present from birth and the adaptive response that is developed over time.
“There are a lot of different types of white blood cells circulating in your blood and tissues,” Fruman said. “Some of them have evolved to recognize commonly–encountered structures on pathogens.”
These cells are part of the innate immune response—the portion of our immune system that we are born with, like a first line of defense—which can recognize and control or eliminate pathogens without requiring prior exposure to them. Fruman said cells like these have evolved receptors in humans that recognize common dangers, but they are non-specific. The innate immune system is pre-existing and ready to rally in the face of a pathogen, but it will not be able to distinguish between two strains of a related virus.
According to Fruman, the adaptive component of immune response takes more time to develop because its cells randomly generate a receptor to recognize particular dangers. This is the portion of the system that does not forget a threat it has seen before.
“This is essentially the basis of all the vaccinations that we administer,” said Bellur Prabhakar, a Ph. D., professor and head of the department of microbiology and immunology and associate dean for research and training programs at the College of Medicine at the University of Illinois Chicago.
Prabhakar said when people are vaccinated against a virus like polio or measles, the immune system creates a memory that allows it to cleanse the body of a virus before it has a chance to take hold. That ability to remember new threats is what differentiates the adaptive from the innate.
“Ultimately, it’s about how the cells generate energy,” Cramer said. “There are a lot of hypotheses about why cells make this switch.”
According to Cramer, what drives the epigenetic change resulting in a metabolic shift in glucose processing that locks the innate immune cells in the trained state is still an open question. Another place this cellular shift from oxidative phosphorylation to aerobic glycolysis is in cancer cells. The change from one method of processing glucose to generate energy in the form of ATP to another may be a way to allow the cells to live in a stressful environment where a critical molecule—oxygen—may be limited.
“There are a lot of drugs in different phases of development targeting HIF1-alpha,” Cramer said. “But because it has so many functions in the cell, it’s unclear if [the gene] could be targeted in this context to do something like improve immune responses in vaccines.”