Roots of near-death experiences explored
Roots of near-death experience explored
May 4, 2015
The experience of imminent death was first described in the 19th century. In recent decades, this concept of the “life review” or “near-death experience” perceived by those poised on the threshold of death has reached the status of cultural trope even though no empirical evidence has established its existence.
A research team led by Jimo Borjigin, an associate professor of molecular & integrative physiology and neurology at the University of Michigan’s Medical School, has published data that seems to pinpoint a biological basis for claims such as “My life flashed before my eyes,” or “I saw a white light at the end of a tunnel.”
“Death is such a grave subject— no one wants to discuss it,” Borjigin said. “It was almost like a dirty word, but there’s huge public interest in near-death experiences.”
Borjigin said that for a long time, both researchers and the public have viewed death as the process of the body shutting down, but a 2013 study she co-authored titled, “Surge of Neurophysiological Coherence and Connectivity in the Dying Brain,” published in the Proceedings of the National Academy of Sciences, found that this is not the case.
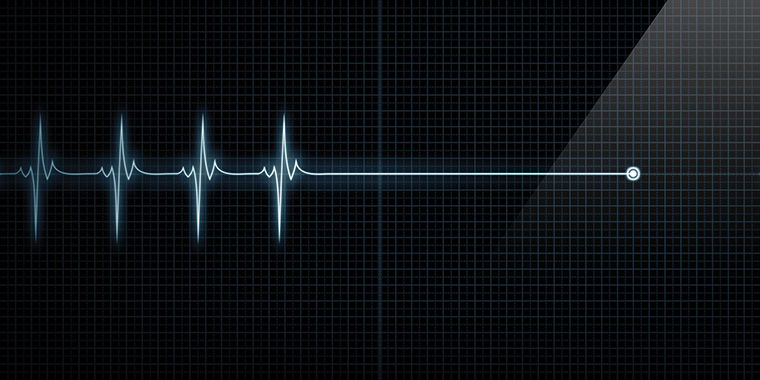
Researchers recorded signs of high-frequency brain waves following cardiac arrest up to the point when patients flatlined. This research may have illuminated the first non-supernatural origins of the near-death experience and why they occur.
Borjigin and her team published the next stage of research on April 6 in the same journal. The paper considers what brain activity physically means in the grand scheme of dying.
In the follow-up study, the researchers induced asphyxia in nine lab mice using carbon dioxide rather than the anesthetic used on mice in the initial study protocol, and monitored the heart and brain with a new device called the electrocardiomatrix. The ECM was developed at the Borjigin laboratory at UM and is like an electrocardiogram but monitors synchronized brain signals and heart rhythms beat-by-beat for periods longer than an hour.
“In previous research, patients were studied solely at the heart,” Borjigin said. “You must look at the brain and heart simultaneously because one has a lethal effect on the other. We are trying to correlate different stages of cardiac failure to what the brain is doing at the time.”
These findings suggest the heart deteriorates further when brain signals to the heart increase.
According to Omar Mabrouk, research investigator of the Kennedy Group at UM, the euphoric perceptions commonly felt as revelations and second chances are most likely due to the excessive release of neurotransmitters during frantic brain-to-heart communication.
“When you have these exaggerated amounts of neurotransmitters, like serotonin, there is a high likelihood that hallucinations would be an outcome,” Mabrouk said. “In addition to having positive moods and altered states of consciousness, there is a whole list of neurochemicals that are associated with mood and cognition.”
This is still under speculation, and further testing at the chemical, cellular and genetic levels are required to see this interplay, but it does seem plausible as to why people have these “realer than real” experiences in these situations, Mabrouk said.
According to the study, more than a dozen neurochemicals were released with increased activation in the left hemisphere and occipital lobe after the heart stopped. Activity occurred at higher frequencies known as gamma oscillations. Borjigin said this asymmetry in brainwave activation is well-researched and referred to as “sidedness”—left- and right-brain traits.
Michael Wang, an assistant professor and director of molecular stroke research at UM, said this asymmetry also plays a role in the autonomic nervous system in humans, where the brain automatically controls functions such as breathing and heartbeat.
“If the brain was just activating because it was distressed, then you might imagine all parts of the brain would be equivalent,” Wang said. “But the fact that there are some specific areas of the brain that are more activated suggest there is some patterning to the process.”
Borjigin and her team also noticed extreme fluctuation in the heart’s rhythm right before cardiac arrest.
“The brain makes even more intense effort in communication to the heart at these times, so we thought maybe the brain suffocated the heart to death,” she said.
From these observations, the researchers decided to see if they could relieve the heart from the bombardment of brain signaling sooner, enabling it to continue functioning for a longer time.
They used a surgical spinal cord transection in the mice, which temporarily blocked specific signals from the brain that burden the heart. The heart was able to beat three times longer in the absence of oxygen once they blocked these signals, Borjigin said.
“We want to find the magic cocktail—the pharmacological mix that can do the same thing or even better,” she said. “Roughly 400,000 people around the nation suffer from sudden cardiac arrest and 90 percent of them die. It’s a high failure rate for medicine if they are unable to resuscitate them.”
Wang said sudden cardiac arrest will always occur, but researchers need to improve the outcomes for patients.
Borjigin and her team want to be able to not only understand the dying process, but eventually find solutions to prevent, delay or revive patients who suffer from cardiac arrest.
“It’s all about figuring out the processes that cause the heart to stop beating, the link between brain signaling and the heart working the way it should,” Mabrouk said. “Maybe some day there could be an injection to prevent a person from slipping past that point where they cannot come back.”