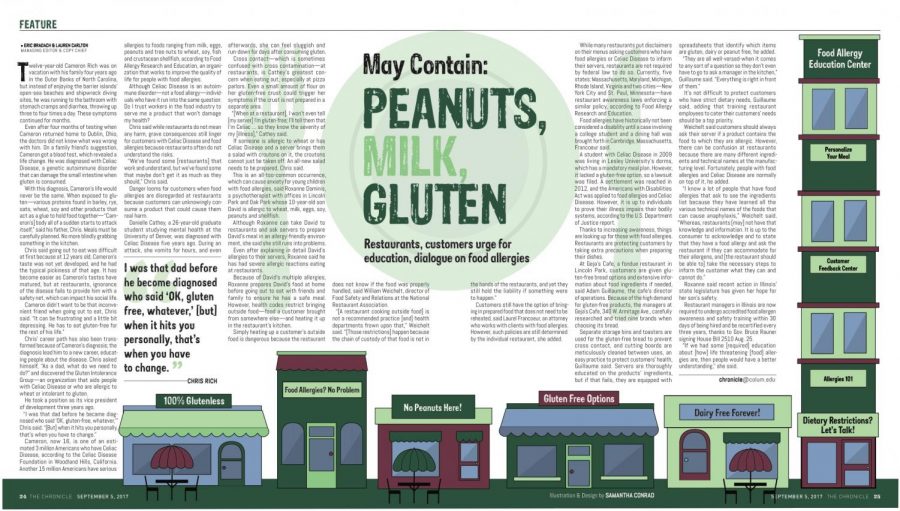
May contain: peanuts, milk, gluten: Restaurants, customers urge for education, dialogue on food allergies
May contain: peanuts, milk, gluten: Restaurants, customers urge for education, dialogue on food allergies
September 5, 2017
Twelve-year-old Cameron Rich was on vacation with his family four years ago in the Outer Banks of North Carolina, but instead of enjoying the barrier islands’ open-sea beaches and shipwreck diving sites, he was running to the bathroom with stomach cramps and diarrhea, throwing up three to four times a day. These symptoms continued for months.
Even after four months of testing when Cameron returned home to Dublin, Ohio, the doctors did not know what was wrong with him. On a family friend’s suggestion, Cameron got a blood test, which revealed a life change. He was diagnosed with Celiac Disease, a genetic autoimmune disorder that can damage the small intestine when gluten is consumed.
With this diagnosis, Cameron’s life would never be the same. When exposed to gluten—various proteins found in barley, rye, oats, wheat, soy and other products that act as a glue to hold food together—“Cameron’s] body all of a sudden starts to attack itself,” said his father, Chris. Meals must be carefully planned. No more blindly grabbing something in the kitchen.
Chris said going out to eat was difficult at first because at 12 years old, Cameron’s taste was not yet developed, and he had the typical pickiness of that age. It has become easier as Cameron’s tastes have matured, but at restaurants, ignorance of the disease fails to provide him with a safety net, which can impact his social life.
Cameron didn’t want to be that inconvenient friend when going out to eat, Chris said. “It can be frustrating and a little bit depressing. He has to eat gluten-free for the rest of his life.”
Chris’ career path has also been transformed because of Cameron’s diagnosis; the diagnosis lead him to a new career, educating people about the disease. Chris asked himself, “As a dad, what do we need to do?” and discovered the Gluten Intolerance Group—an organization that aids people with Celiac Disease or who are allergic to wheat or intolerant to gluten.
He took a position as its vice president of development three years ago.
“I was that dad before he became diagnosed who said ‘OK, gluten-free, whatever,’” Chris said. “[But] when it hits you personally, that’s when you have to change.”
Cameron, now 16, is one of an estimated 3 million Americans who have Celiac Disease, according to the Celiac Disease Foundation in Woodland Hills, California. Another 15 million Americans have serious allergies to foods ranging from milk, eggs, peanuts and tree nuts to wheat, soy, fish and crustacean shellfish, according to Food Allergy Research and Education, an organization that works to improve the quality of life for people with food allergies.
Although Celiac Disease is an autoimmune disorder—not a food allergy—individuals who have it run into the same question: Do I trust workers in the food industry to serve me a product that won’t damage my health?
Chris said while restaurants do not mean any harm, grave consequences still linger for customers with Celiac Disease and food allergies because restaurants often do not understand the risks.
“We’ve found some [restaurants] that work and understand, but we’ve found some that maybe don’t get it as much as they should,” Chris said.
Danger looms for customers when food allergies are disregarded at restaurants because customers can unknowingly consume a product that could cause them real harm.
Danielle Cathey, a 26-year-old graduate student studying mental health at the University of Denver, was diagnosed with Celiac Disease five years ago. During an attack, she vomits for hours, and even afterwards, she can feel sluggish and run-down for days after consuming gluten.
Cross contact—which is sometimes confused with cross contamination—at restaurants, is Cathey’s greatest concern when eating out, especially at pizza parlors. Even a small amount of flour on her gluten-free crust could trigger her symptoms if the crust is not prepared in a separate area.
“[When at a restaurant], I won’t even tell [my server] I’m gluten-free; I’ll tell them that I’m Celiac … so they know the severity of my [illness],” Cathey said.
If someone is allergic to wheat or has Celiac Disease and a server brings them a salad with croutons on it, the croutons cannot just be taken off: An all-new salad needs to be prepared, Chris said.
This is an all-too-common occurrence, which can cause anxiety for young children with food allergies, said Roxanne Dominis, a psychotherapist with offices in Lincoln Park and Oak Park whose 10-year-old son David is allergic to wheat, milk, eggs, soy, peanuts and shellfish.
Although Roxanne can take David to restaurants and ask servers to prepare David’s meal in an allergy-friendly environment, she said she still runs into problems.
Even after explaining in detail David’s allergies to their servers, Roxanne said he has had severe allergic reactions eating at restaurants.
Because of David’s multiple allergies, Roxanne prepares David’s food at home before going out to eat with friends and family to ensure he has a safe meal. However, health codes restrict bringing outside food—food a customer brought from somewhere else—and heating it up in the restaurant’s kitchen.
Simply heating up a customer’s outside food is dangerous because the restaurant does not know if the food was properly handled, said William Weichelt, director of Food Safety and Relations at the National Restaurant Association.
“[A restaurant cooking outside food] is not a recommended practice [and] health departments frown upon that,” Weichelt said. “[Those restrictions] happen because the chain of custody of that food is not in the hands of the restaurants, and yet they still hold the liability if something were to happen.”
Customers still have the option of bringing in prepared food that does not need to be reheated, said Laurel Francoeur, an attorney who works with clients with food allergies. However, such policies are still determined by the individual restaurant, she added.
While many restaurants put disclaimers on their menus asking customers who have food allergies or Celiac Disease to inform their servers, restaurants are not required by federal law to do so. Currently, five states: Massachusetts, Maryland, Michigan, Rhode Island, Virginia and two cities—New York City and St. Paul, Minnesota—have restaurant awareness laws enforcing a similar policy, according to Food Allergy Research and Education.
Food allergies have historically not been considered a disability until a case involving a college student and a dining hall was brought forth in Cambridge, Massachusetts, Francoeur said.
A student with Celiac Disease in 2009 was living in Lesley University’s dorms, which has a mandatory meal plan. However, it lacked a gluten-free option, so a lawsuit was filed. A settlement was reached in 2012, and the Americans with Disabilities Act was applied to food allergies and Celiac Disease. However, it is up to individuals to prove their illness impairs their bodily systems, according to the U.S. Department of Justice report.
Thanks to increasing awareness, things are looking up for those with food allergies. Restaurants are protecting customers by taking extra precautions when preparing their dishes.
At Geja’s Cafe, a fondue restaurant in Lincoln Park, customers are given gluten-free bread options and extensive information about food ingredients if needed, said Adam Guillaume, the cafe’s director of operations. Because of the high demand for gluten-free products, the managers at Geja’s Cafe, 350 W. Armitage Ave., carefully researched and tried nine brands when choosing its bread.
Separate storage bins and toasters are used for the gluten-free bread to prevent cross contact, and cutting boards are meticulously cleaned between uses, an easy practice to protect customers’ health, Guillaume said. Servers are thoroughly educated on the products’ ingredients, but if that fails, they are equipped with spreadsheets that identify which items are gluten, dairy or peanut free, he added.
“They are all well-versed-when it comes to any sort of a question so they don’t even have to go to ask a manager in the kitchen,” Guillaume said. “Everything is right in front of them.”
It’s not difficult to protect customers who have strict dietary needs, Guillaume said, adding that training restaurant employees to cater their customers’ needs should be a top priority.
Weichelt said customers should always ask their server if a product contains the food to which they are allergic. However, there can be confusion at restaurants because there are many different ingredients and technical names at the manufacturing level. Fortunately, people with food allergies and Celiac Disease are normally on top of it, he added.
“I know a lot of people that have food allergies that ask to see the ingredients list because they have learned all the various technical names of the foods that can cause anaphylaxis,” Weichelt said. “Whereas, restaurants [may] not have that knowledge and information. It is up to the consumer to acknowledge and to state that they have a food allergy and ask the restaurant if they can accommodate for their allergens, and [the restaurant should be able to] take the necessary steps to inform the customer what they can and cannot do.”
Roxanne said recent action in Illinois’ state legislature has given her hope for her son’s safety.
Restaurant managers in Illinois are now required to undergo accredited food allergen awareness and safety training within 30 days of being hired and be recertified every three years, thanks to Gov. Bruce Rauner signing House Bill 2510 Aug. 25.
“If we had some [required] education about [how] life threatening [food] allergies are, then people would have a better understanding,” she said.