Appetite-controlling hunger neuron influences white fat ‘browning’
October 20, 2014
Standing outside in frigid temperatures is one way to access the type of fat in the human body that generates heat to help protect itself from the cold.
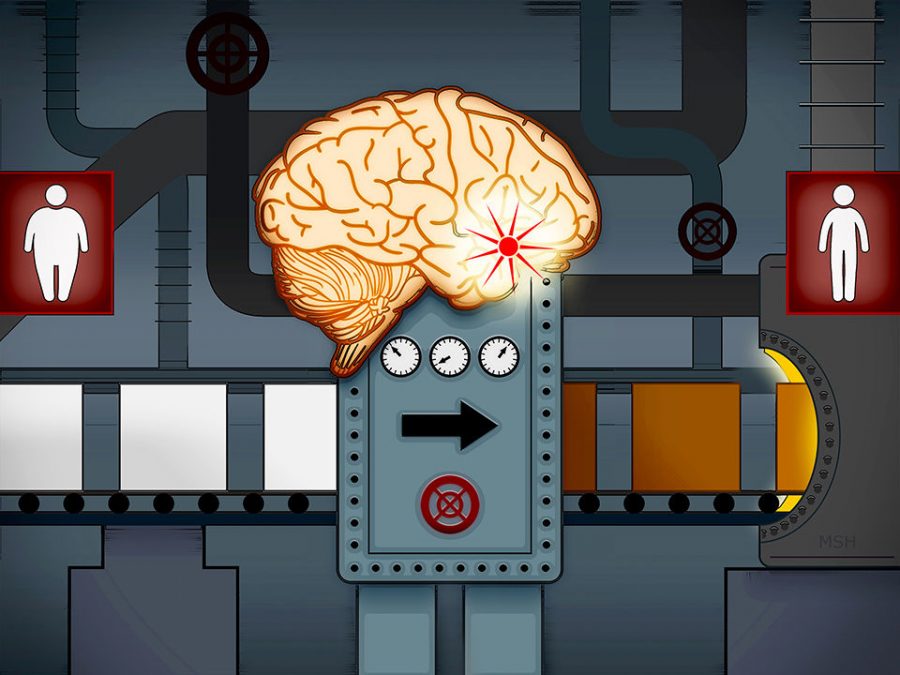
While it has been known for some time that white fat, which stores fat as energy, can transform into brown fat—which burns stored energy and generates heat, causing weight loss—under conditions such as exposure to cold temperatures or hunger, how these processes are controlled in the brain has been less clear. Researchers from Yale University School of Medicine have identified a process in the brain that may hold promise for the treatment of conditions such as obesity and diabetes.
“We found that the brain actually plays a key role in controlling the browning [of white fat] and prevented the mice from becoming obese,” said Xiaoyong Yang, co-author of the study and associate professor of Comparative Medicine and Cellular and Molecular Physiology at Yale School of Medicine.
In the study, published Oct. 9 in the journal Cell, researchers identified the hunger neuron in the brain that controls the conversion of white fat into brown fat and improves energy metabolism. This hunger neuron can be activated through fasting, which acts as a signal to allow the brain to control the fat-burning process.
“We found that the molecular pathway of the hunger neuron was critical to [controlling its] activity in response to fasting,” Yang said. “This is like the molecular switch that could turn [the neuron] on and off depending on whether or not you eat or starve.”
According to Tamas Horvath, chair of the Comparative Medicine Department at Yale School of Medicine and co-author of the Cell study, the body registers hunger when the neurons in the brain that control hunger are active. The neurons seem to be suppressing the sympathetic nervous system, which sends signals from the brain to the periphery of the nervous system, including fat cells.
“If you use various means to stop these cells from functioning, then the sympathetic nervous system [is] activated and the peripheral white fat turns into brown and you start to burn more energy,” Horvath said. “The conclusion is that if you put these[rats] on calorie-dense diets, they don’t gain as much weight because it’s burned as heat.”
According to Labros Sidossis, director of the Metabolism Unit at the Shriners Hospital for Children in Galveston, Texas, some mitochondria have specialized proteins that instead of producing ATP—the way cells use energy in the human body—produce heat. The types of mitochondria that have these properties are capable of accessing BAT.
“[Heat] is actually the only way for a cell to dissipate energy,” Sidossis said. “So what makes the BAT different from WAT is that BAT is very rich in mitochondria that have those specialized proteins.”
The researchers from the Cell study also focused on the effects of cold exposure and fasting on the browning of WAT. Horvath said the type of fat the body accesses for energy use depends on the energetic state it is in at the time.
“If you’ve had a lot of food and you’re full, then you’re going to store fat, but you’re also in the position to burn it because you have excess energy,” Horvath said. “Cold exposure and hunger are very similar in the sense of needing to move to ‘reserve mode,’ but hunger basically overrides cold exposure.”
Shivering outside on that cold winter day may be a way to burn excess calories as heat unless it is on an empty stomach. In this energy-deprived state, rather than expending valuable stored energy to keep itself warm, the body will conserve energy by deactivating its fatty tissue reserves. Horvath said the cold exposure might activate the browning of white fat, but being in a fasted state turns can inhibit that change.
“You could imagine that if you [added these factors to] your lifestyle—skipping food every two days or keeping the heat turned off in your home—your metabolic profile would benefit from it,” he said.
In a July 23 study published in the journal Diabetes, Sidossis and colleagues from the Shriners Hospital for Children revealed for the first time in humans that those with brown fat are more capable of regulating their blood sugar and the tissue may have an anti-diabetic function in humans.
“If someone has brown fat or was able to somehow increase the brown fat content in their body, they would probably be able to prevent or treat insulin resistance and diabetes,” Sidossis said.
Study participants were placed in a room for a prolonged period of time with temperatures ranging from 67–69 degrees Fahrenheit. This was cold enough to activate their BAT and allow researchers to measure the way the body regulated their metabolisms.
“We came to the conclusion that if you have brown fat and are able to activate it, this tissue would absorb glucose circulating in the blood in order to burn it and preserve heat,” Sidossis said. “Blood sugar levels would decrease. It would function like drugs or insulin that diabetics take to regulate their blood sugar.”